Varicose Veins
What causes Varicose veins?
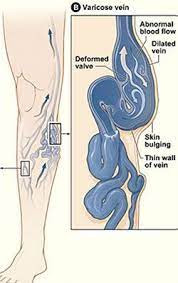
Related risk factors are multiple, including primary etiologies associated with pregnancy, prolonged standing, female gender, and, rarely, congenital absence of valves. In addition, varicosities may develop as a result of prior DVT or trauma. Valve failure may be primary and occur as a result of pre existing weakness in the vessel wall or valve leaflets causing increase in venous pressure and return of blood is impaired. Genetic Predisposition .
The risk of varicose veins’ developing was 90% if both parents were affected, 25% for males and 62% for females if one parent was affected, and 20% if neither parent was affected.
Is Varicose Veins Preventable?
Varicose veins constitute a progressive disease; remission of the disease does not occur, except after pregnancy and delivery. Even though non operative management of venous disease, including compression, elevation, and skin care, is clearly beneficial, such therapy does not correct the underlying pathology, allows immediate recurrence of symptoms if patients are unable to comply with the elevation and compression regimen, and is associated with a high incidence of recurrent ulceration and progression of disease.


What are the Symptoms of Varicose Veins?
The manifestations of Varicose veins can be different and most common signs are related to appearance of telangiectasias, reticular veins, varicose veins, lipodermatosclerosis, and venous ulcers. The pain or discomfort of the leg is typically described as heaviness or aching aggravated by prolonged standing and relieved by elevation. Swelling, ulceration of the legs, Venous-related skin changes may also develop, including hyperpigmentation, eczematous dermatitis, cellulitis, and lymphangitis.
Does of Compression Therapy Helps?
The non operative approach to patients with chronic venous disease includes lifestyle modification, compression, and pharmacologic therapies. The rationale of graded external compression is to oppose the main pathogenetic factor underlying chronic venous disease, reflux-induced venous hypertension, and Compression therapy has also been shown to improve venous pump function, enhances lymphatic drainage and cutaneous oxygenation as demonstrated by increased transcutaneous tissue oxygen saturation levels. The improved cutaneous microcirculatory environment has been thought to promote venous ulcer healing.
However, use of compression stockings was not shown to prevent disease progression or recurrence of varicose veins after treatment. The recommendation for use of class 2 compression stockings in uncomplicated symptomatic varicose veins is also weak (grade 2B) and only for symptom relief of leg swelling and not curative.


